Abstract
Background
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, clonal disorder of hematopoietic stem cells, characterized by complement-mediated intravascular hemolysis, thrombosis, and bone marrow failure. Pregnancy exacerbates the clinical features of PNH, increasing maternal and fetal morbidity and mortality. Pregnancy in patients with PNH has traditionally been discouraged.
Terminal complement inhibition with eculizumab gained regulatory approval in 2007 and has revolutionized the management of PNH. Limited data suggest that eculizumab is also safe and efficacious during pregnancy. Owing to the rarity of PNH and the inability to conduct randomized controlled trials on this population, most reports are small case series, with even the largest retrospective studies including well below 100 patients.
We therefore present the first comprehensive systematic review and meta-analysis of outcomes in 190 pregnancies from 135 women with PNH. We compare pregnancy complications between those receiving eculizumab and those not, since complement blockade is not universally available. For the first time we demonstrate that eculizumab is associated with a lower risk of fetal loss.
Methods
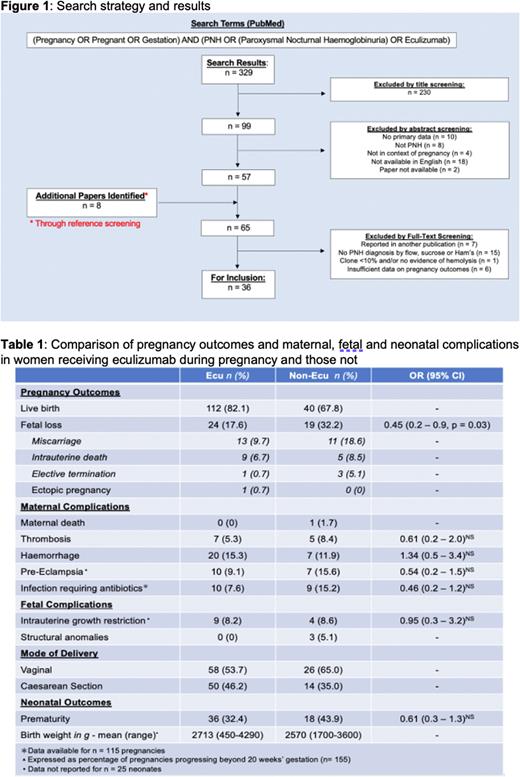
The PubMed (Medline) database was searched for studies reporting primary data on pregnancy outcomes in the context of classical hemolytic PNH, diagnosed through flow cytometry, acid Ham's or sucrose lysis (Figure 1). Women with evidence of recurrent hemolytic episodes including serum lactate dehydrogenase >1.5 times the upper limit of normal, and typical PNH symptoms were included. We excluded papers where there was insufficient information for meaningful downstream analysis, or where cases were duplicated elsewhere in the literature. The search was restricted to English language papers. Two reviewers independently screened articles for inclusion with a third opinion sought where there was disagreement. References of included papers and review articles were screened to identify further papers.
Thirty-six papers published between 1968 to 2021 were selected for inclusion. The majority were small case series or single case studies. There were two larger retrospective studies reporting on 45 and 75 pregnancies respectively. There was one prospective study (n=15 pregnancies).
Results
Eculizumab was used in 130 pregnancies. No maternal deaths were reported in patients on eculizumab. One woman who had never received eculizumab died at 12 weeks postpartum from intra-abdominal sepsis following a severe episode of acalculous cholecystitis. A higher rate of fetal survival was observed in pregnancies where eculizumab was used (82%) than in pregnancies when it was not (69%) (Table 1). Thrombosis occurred at a higher rate than in the healthy pregnant population but did not significantly differ in incidence between treatment groups (Table 1). The incidence of pre-eclampsia was high in this population. There was a trend towards a reduced risk of pre-eclampsia and infection in eculizumab pregnancies, but this did not reach statistical significance (Table 1). No Neisserial infections were observed in patients treated with eculizumab.
The rate of spontaneous miscarriage (<24 weeks') was nearly twice as high in women who had not received eculizumab (18.6%) compared to those who received it (9.7%). The rate of intrauterine death did not significantly differ between treatment groups (Table 1). Fetal structural anomalies occurred in three cases, none of which had been exposed to eculizumab, supporting the notion that the drug does not have a teratogenic effect. Intrauterine growth restriction (IUGR) occurred in just over 8% of pregnancies that progressed beyond 20 weeks and did not differ between treatment groups (Table 1). IUGR was associated with pre-eclampsia in eight cases (61%).
148 pregnancies progressed to delivery, the majority by vaginal delivery. Premature birth (<37 weeks' gestation) was observed in 32% of eculizumab pregnancies and 44% of non-eculizumab pregnancies. Premature delivery was usually iatrogenic due to maternal or fetal complications, with spontaneous premature labor in only eight cases (15%).
Conclusion
Eculizumab appears to be safe and provide a benefit in pregnancy in PNH. There were less premature births and spontaneous miscarriages and greater fetal survival when eculizumab was given. A tendency to fewer cases of pre-eclampsia and maternal infections was also seen.
Disclosures
Griffin:Sobi Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Alexion: Honoraria, Other: Conference support; BioCryst Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Medscape: Other: educational work sponsored by Apellis with unrestricted grant paid to Medscape. Kelly:Medscape: Other: educational work sponsored by Apellis with unrestricted grant paid to Medscape; Swedish Orphan Biovitrum AB: Membership on an entity's Board of Directors or advisory committees; Alexion: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: conference support; Biocryst: Membership on an entity's Board of Directors or advisory committees; Sobi: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees; Biologix: Research Funding; Jazz: Membership on an entity's Board of Directors or advisory committees, Research Funding; Astellas: Research Funding; Amgen: Consultancy.
OffLabel Disclosure:
Eculizumab is a monoclonal antibody that inhibits terminal complement formation. It is licensed for the management of paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, myasthenia gravis and neuromyelitis optica spectrum disorder. It is not licensed for the treatment of pregnant patients, but has been used off-label for this indication.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal